
 Tc99m Depreotide Scan (NeoTect): Small cell lung cancer in the left lower lobe with possible metastatic left axillary lymph node. There is some more subtle mediastinal activity as well.
Tc99m Depreotide Scan (NeoTect): Small cell lung cancer in the left lower lobe with possible metastatic left axillary lymph node. There is some more subtle mediastinal activity as well.
 Tc99m Depreotide Scan (NeoTect): Small cell lung cancer in the left lower lobe with possible metastatic left axillary lymph node. There is some more subtle mediastinal activity as well.
Tc99m Depreotide Scan (NeoTect): Small cell lung cancer in the left lower lobe with possible metastatic left axillary lymph node. There is some more subtle mediastinal activity as well. Click on Image for Larger View
Click on Image for Larger View CT chest: Type A Aortic disection with rupture into pericardial space. Note the intimal flap in the ascending aorta and the intermediate density blood in the pericardial space.
CT chest: Type A Aortic disection with rupture into pericardial space. Note the intimal flap in the ascending aorta and the intermediate density blood in the pericardial space. Scan classification showing blood-pool phase at top and delayed phase at bottom: focal hyperemia in plantar fascia and marked delayed uptake in inferior calcaneum (A), hyperemia in proximal third and mild delayed uptake (B), and diffuse hyperemia and moderate delayed uptake (C). Arrowheads indicate hyperemia; arrows indicate delayed uptake. Copyright © 2006 by the Society of Nuclear Medicine.
Scan classification showing blood-pool phase at top and delayed phase at bottom: focal hyperemia in plantar fascia and marked delayed uptake in inferior calcaneum (A), hyperemia in proximal third and mild delayed uptake (B), and diffuse hyperemia and moderate delayed uptake (C). Arrowheads indicate hyperemia; arrows indicate delayed uptake. Copyright © 2006 by the Society of Nuclear Medicine.I thought this might be of interest to Podiatry Residents who rotate through.
Source: Shalmali Pal. AuntMinnie.com staff writerOctober 25, 2006
In an earlier post I mentioned Amide as a nice freeware for image fusion. I should give equal time to MIM. This CLEVELAND based company founded by Dennis Nelson PhD makes terrific visualization software for nuclear imaging and medical imaging in general. It is actually what we use most for daily PET/CT reading. The reason is that it is very intuitive and does a great job streamlining PET /CT work flow. They are also doing a great job integrating their software with PACS systems.
 Click image for full size
Click image for full size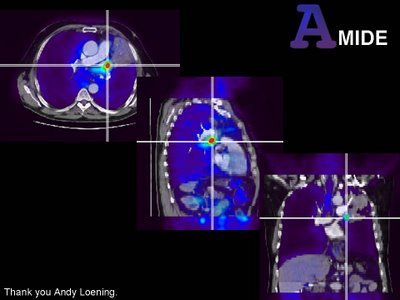 Click image for full size
Click image for full size Click image for full size
Click image for full size (Click image for full size)
(Click image for full size)Image A and D: Coronal and axial T2 fat supressed MRI of lower extremities in a 14m old male infant. Note the large perineal lymphatic mass extending upinto the pelvis. Also near the knees there are other vascular / lymphatic malformations.
Image B: Image fusion of contrast MRA with conventional T2 MRI in volume rendering. You can now see the full exrtent of the vascular / lymphatic malformations in 3D with ther relationship to the arteries. Note the limited visualization of lower extremity arteries in the left calf. Patients with KT syndrome can have arterial abnormalities including atresias in the lower extremities.
Image D: Fusion of MR venogram with T2 coronal images in volume rendering. Tee entire deep venous system has been replaced by extensive collaterals. The large lateral venous channels in the thighs are called Trenaunay veins.

All of our 3D/VR models of pathology are here here at the top of the site. They will remain there permanently. There are currently 70+ mod...